
14 Sep Masks: The Covid19 Talisman
Over the last six months I’ve wondered why masks have been recommended? Mask wearing in public areas has been mandated by Governors and supported by the media. Biosafety and the fear created by public officials has pushed this agenda and without ever giving any scientific support. In fact, at the outset of the “Covid19 pandemic” there were conflicting opinions about mask wearing with the Surgeon General of the U.S. stating that masks were not necessary for healthy individuals. This I thought was reasonable. Masks (and quarantine) are for sick people. In thirty years of practice (and contact with 500 patients per month) I have never worn a mask during any pandemic. Fastidious hand-washing before and after every patient contact has always worked. Also, if sick, you stay home. Common sense.
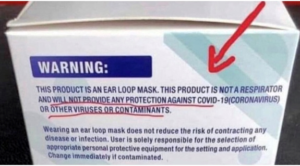
So why all the fuss and government control over a Coronavirus? Is this virus different in some way? We’ve never been “mandated” by the government to wear masks in the past, why now? Could government officials and technocrats be wrong? They certainly were very wrong on their predictions. Remember on March 30th, the now infamous Imperial College London model predicted 2.2 million deaths in the U.S. by September 1st. The most recent numbers given by the CDC are that 9,210 people have died from Covid19. Among other things, our government “experts” failed to distinguish between dying “from” Covid19 and dying “with” Covid19. If masks are truly effective, why did we have quarantine and a shutdown? If masks work, why the “social distancing”? If masks work, why weren’t they given to residents of nursing homes preventing thousands of deaths? If Covid19 is so contagious why are we not required to dispose of masks in a biohazard container? If masks work, why is there a disclaimer on the side of the box stating it “will not provide any protection against Covid19 (coronavirus)”? Is there an agenda or is this purely incompetence on the part of public officials? What’s really going on here?
So are masks effective?
In short, no. Two meta-analysis studies found that masks have no detectable effect against transmission of viral infections. Compared to no masks, there was no reduction of influenza-like illness cases or influenza for masks in the general population, nor in healthcare workers (1). A recent study from the University of Hong Kong found that evidence from randomized controlled trials of face masks did not support a substantial effect on transmission of laboratory-confirmed influenza, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility (2). What about the N95 masks? A study of 2862 individuals showed that both N95 respirators and surgical masks resulted in no significant difference in the incidence of laboratory confirmed influenza (3). 2011 and 2016 meta-analysis studies of mask use had similar results finding no conclusive relationship between mask/N95 respirator use and protection against influenza infection (4,5). Furthermore a 2008 study of face mask use in health care workers did not demonstrate a benefit to protect against cold symptoms or contracting a cold (6).
What about airflow around a mask and penetration through a mask? Does the seal around cloth masks, surgical masks and N95 masks truly provide protection to the user and those around? All masks are thought to block forward air flow by 90%. Do your eye glasses fog when you wear a mask? Unless the mask has an adhesive seal over the nose your eye glasses are going to fog. This is evidence of brow jets (unfiltered upward airflow past eyebrows) and Schlieren imaging has shown that both surgical masks and cloth masks have further and larger brow jets than not wearing a mask at all (7). So with the use of a mask your eyes (eye glasses) are being contaminated with virus infested breath when exhaling. Backward unfiltered airflow is also very strong compared to not wearing a mask. So exhaled air along with the virus is going to escape behind the mask wearer and above via brow jets. Forward protection is no better. A study by Jung et al tested 44 different brands of masks finding a mean 35.6% penetration and medical masks, general masks and handkerchiefs were found to provide little protection against respiratory aerosols (8). Penetration through cloth masks is 97% and through medical masks is 44% (9). Your exhaled breath is hindered by a mask and escapes through the mask along with being deflected above the mask (brow jet) and backwards offering no benefit (protection) to those around you.

An editorial from the New England Journal of Medicine commenting on the topic of mask use versus Covid19 assesses the matter as follows:
“We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 20 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.” (10).
Further, Klompas et al state, “What is clear, however, is that universal masking alone is not a panacea… Focusing on universal masking alone may, paradoxically, lead to more transmission of Covid-19 if it diverts attention from implementing more fundamental infection-control measures.” (10).
Are N95 respirators, surgical masks and cloth masks safe?
Mask wearing brings up concerns about burdening the circulatory and immune systems. Some feel that with the use of a mask and oxygen reduction, hypercapnia may cause cardiac overload, renal overload and a shift to metabolic acidosis.
Studies have shown that 19% of patients developed various degrees of hypoxia and oxygen consumption was reduced by 13.8% in healthcare workers compared to controls and personal bioaerosol samplers confirmed the harboring of influenza virus in N95 masks (11, 12, 13). Surgical masks and cloth masks are no better and may be worse.
Surgical masks worn by healthcare workers were shown to harbor influenza virus and healthcare workers using cloth masks had significantly higher rates of influenza-like illness after four weeks of on-the-job use when compared to controls (13, 14). Daily and long-term use of masks may exacerbate Covid19.
Cloth masks, surgical masks, N95 masks, bandanas and scarves offer poor protection to aerosolized pathogens. The use of a mask allows transmission of aerosolized pathogens in various directions (up and behind the wearer) and permits self-contamination. In Europe, the Danish people do not wear masks and according to Johns Hopkins University boast one of the lowest Covid19 death rates in the world. It’s time to rid ourselves of the mask talisman.
1) T Jefferson, M Jones, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 1 – Face masks, eye protection and personal distancing: systemic review and meta-analysis. MedRxiv. 2020.
https://www.medrxiv.org/content/10.1101/2020.03.30.20047217v2
2) J Xiao, E Shiu, et al. Nonpharmaceutical measures for pandemic influenza in non-healthcare settings – personal protective and environmental measures. Centers for Disease Control. 2020; 26(5).
https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
3) L Radonovich M Simberkoff, et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinic trial. JAMA. 2019; 322(9): 824-833.
https://jamanetwork.com/journals/jama/fullarticle/2749214
4) J Smith, C MacDougall. CMAJ. 2016 May; 188(8); 567-574.
https://www.cmaj.ca/content/188/8/56
5) F bin-Reza, V Lopez, et al. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence. 2012; 6(4): 257-267.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779801/
6) J Jacobs, S Ohde, et al. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am J Infect Control. 2009; 37(5): 417-419.
https://pubmed.ncbi.nlm.nih.gov/19216002/
7) M Viola, B Peterson, et al. Face coverings, aerosol dispersion and mitigation of virus transmission risk.
https://arxiv.org/abs/2005.10720, https://arxiv.org/ftp/arxiv/papers/2005/2005.10720.pdf
8) H Jung, J Kim, et al. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 2013; 14:991-1002.
https://aaqr.org/articles/aaqr-13-06-oa-0201.pdf
9) C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577.long
10) M Klompas, C Morris, et al. Universal masking in hospitals in the Covid-19 era. N Eng J Med. 2020; 382 e63.
https://www.nejm.org/doi/full/10.1056/NEJMp2006372
11) T Kao, K Huang, et al. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004; 103(8):624-628.
https://pubmed.ncbi.nlm.nih.gov/15340662/
12) P Shuang Ye Tong, A Sugam Kale, et al. Respiratory consequences of N95-type mask usage in pregnant healthcare workers – A controlled clinical study. Antimicrob Resist Infect Control. 2015; 4:48.
https://pubmed.ncbi.nlm.nih.gov/26579222/
13) F Blachere, W Lindsley et al. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J Viro Methods. 2018; 260:98-106.
https://pubmed.ncbi.nlm.nih.gov/30029810/
14) C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577

