20 May Subluxing Peroneal Tendons
Subluxing or dislocating peroneal tendons are a relatively uncommon condition. Patients will complain about the tendons on the outside of the ankle “popping out” or snapping when rotating their ankle. Patients will often complain of a weak ankle on the involved side stating their ankle gives way and they feel the ankle is weak. The peroneal tendons sit in a thick fibrocartilaginous periosteal cushioned groove and if the groove is not deep enough or if the periosteal ridge is absent the tendons can slide out. If a ligament known as the superior peroneal retinaculum is absent, thin or has a loose attachment to the fibula the peroneal tendons may also slide out. One or both of these issues may be present as the cause.

Disruption of the lateral collateral ankle ligaments places considerable strain on the superficial peroneal retinaculum. So much so that at times subluxation is associated with longitudinal splits to the peroneus brevis tendon. This explains how these two conditions commonly coexist. With recurrent peroneal tendon subluxation patients will give a history of previous ankle sprains and injury and this may be misdiagnosed as a simple ankle sprain. Along with the unstable ankle, patients may have popping or a snapping sensation about the outside of the ankle while walking. Obtaining an MRI of the area is a debated issue as the diagnosis and management of subluxing peroneal tendons with lateral ankle instability is based on clinical evidence.
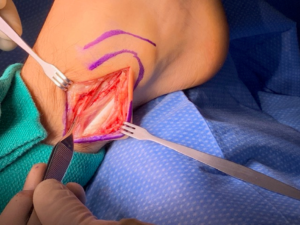
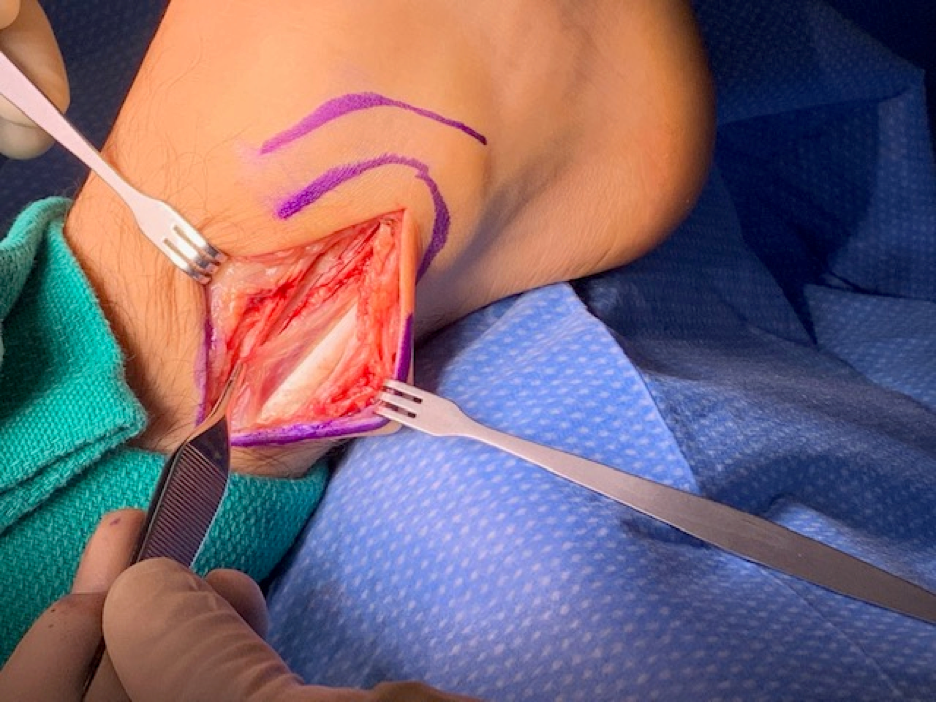
Very little successful conservative (nonsurgical) treatment exists for subluxing peroneal tendons with lateral ankle instability. Recurrent dislocations should be managed with surgical reconstruction. Five basic surgical repair categories have been described in the literature: (i) anatomical reattachment of the superior peroneal retinaculum, (ii) bone-block procedures, (iii) reinforcement of the superior peroneal retinaculum with local tissue transfers (advancement of a portion of the achilles tendon), (iv) rerouting the tendons behind the calcaneofibular ligament and (v) various fibular groove deepening procedures. Your foot and ankle surgeon will determine the procedures best suited for you based on your symptoms and the surgeons experience with this pathology.

Recovery after surgical reconstruction will depend on the procedures performed. On average patient will be nonweightbearing in a pneumatic fracture boot using crutches for four weeks followed by four more weeks of weightbearing in a pneumatic fracture boot. By eight weeks after surgery your surgeon may transfer you to an ankle brace with athletic shoe wear and begin physical therapy including range of motion exercises, strength, and gait training. Patient will return to full function and many patients comment that the operative ankle “now feels stronger” than the other side.
Dr. Strash is double board certified. He is board-certified in Foot Surgery along with being board certified in Rearfoot Reconstructive Ankle Surgery by the American Board of Foot and Ankle Surgery. With nearly thirty years of practice experience, he can help. Remember, at Strash Foot and Ankle Care, we’re here to help you put your best foot forward again!

